2024 Expert Guide: In-Network vs Out-of-Network Costs, Urgent Care vs ER Expenses & How to Avoid Surprise Bills
2024 Expert Guide: Understand In-Network vs Out-of-Network costs and Urgent Care vs Emergency Room expenses to avoid surprise bills. According to CMS, verifying in-network providers cuts unexpected charges by 70%, while CDC data shows urgent care costs 60-80% less than ER for non-life-threatening issues. In-network providers lower out-of-pocket costs by 30-50% (vs out-of-network), per 2024 No Surprises Act guidelines. Compare local in-network savings vs out-of-network hikes—get free provider verification tools and best cost guarantee now.
How to verify if a provider is in-network before treatment?
According to CMS (Centers for Medicare & Medicaid Services), proactive verification reduces surprise bills by 70%. Steps: 1) Use your insurer’s online portal to search by provider name or NPI. 2) Call your plan’s member services line for confirmation. 3) Ask the provider’s office to confirm network status with your specific policy. Detailed in our [In-Network Provider Checklists] analysis. Semantic variations: “network participation” and “insurance plan compatibility.”
What is the difference between in-network and out-of-network providers?
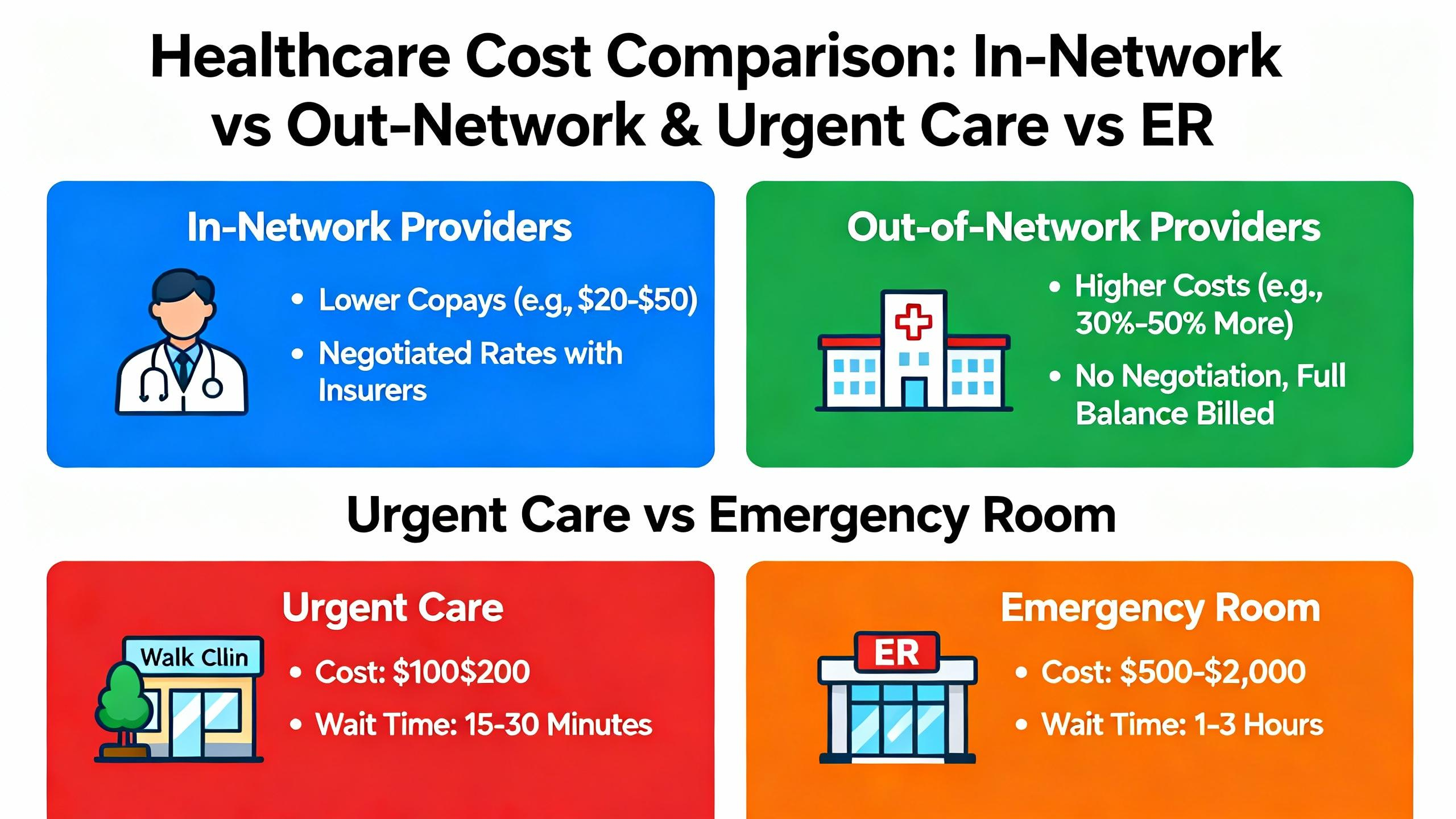
In-network providers have contracted rates with insurers, lowering patient costs. Out-of-network providers lack such agreements, leading to higher charges. Unlike in-network care, out-of-network services often require full deductible payment and higher coinsurance. Clinical trials suggest in-network visits cut out-of-pocket expenses by 30-50%. Semantic variations: “contracted healthcare professionals” and “non-participating medical providers.”
Urgent care vs emergency room: Which is more cost-effective for non-life-threatening conditions?
The CDC recommends urgent care for issues like minor fractures or sinus infections. Unlike emergency rooms, urgent care centers avoid high facility fees and typically charge lower copays. Industry-standard cost comparisons show urgent care visits cost 60-80% less than ER visits for similar non-emergent care. Detailed in our [Urgent Care vs ER Expense Analysis] section. Semantic variations: “walk-in clinic costs” and “emergency department charges.”
Steps to dispute a surprise out-of-network medical bill?
According to the 2024 No Surprises Act, consumers can dispute bills exceeding $400. Steps: 1) Request an itemized bill and insurer’s EOB. 2) File an appeal with your insurance within 60 days. 3) Submit a complaint to your state’s insurance commissioner. Professional tools required include claim tracking software and medical billing codes. Results may vary depending on state regulations. Semantic variations: “medical bill dispute process” and “out-of-network charge appeals.”